
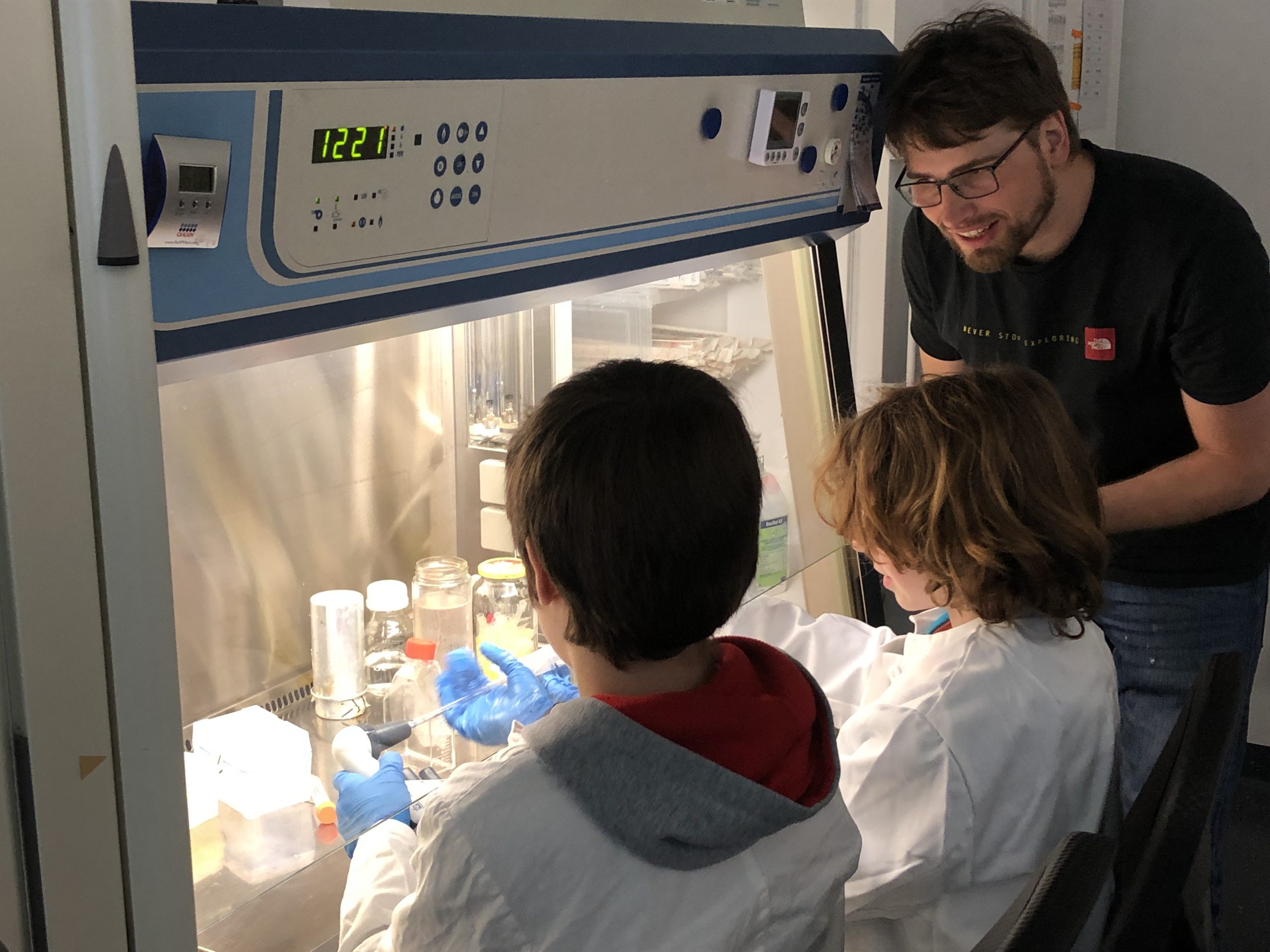
20 Kinder verbrachten am 25.04.2024 einen aufregenden Zukunftstag im Niedersächsischen Zentrum für Biomedizintechnik und Implantatforschung, wo sie faszinierende Einblicke in die Welt der Implantatforschung erhielten. So lernten die Schüler*innen unter anderem wie Zellen tauben Patienten helfen können, das Licht in die Zelle kommt und wie Blut besser konserviert werden kann. Wie im letzten Jahr konnten wir auch dieses Mal wieder ein Angebot für ukrainische Schüler bereitstellen. Es war eine inspirierende Erfahrung für alle Beteiligten!





From Bärbel Hilbig
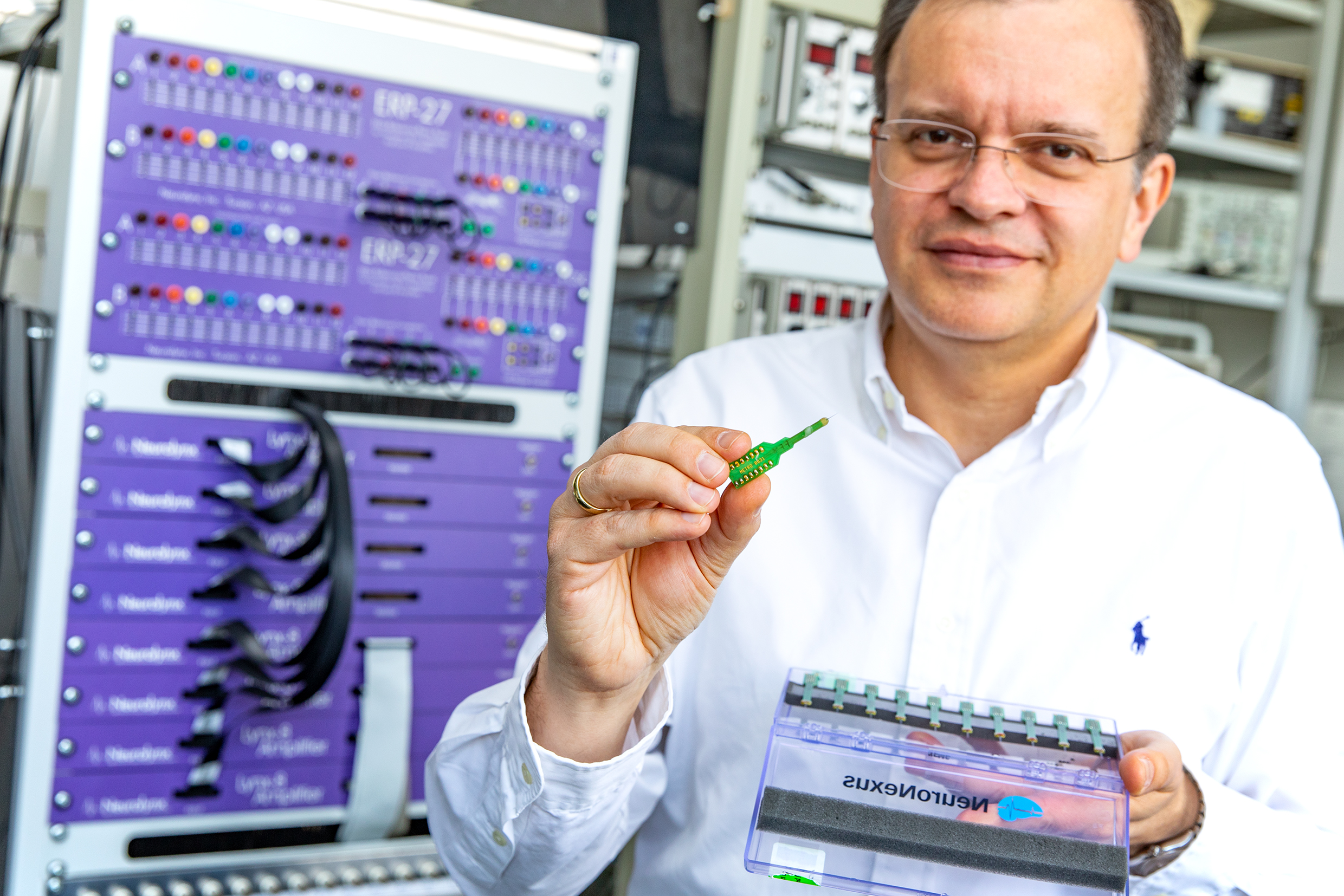
People with hearing problems are quickly isolated, cut off from conversations, also because those around them may not even be aware of their impairment. How hearing impaired people can hear again or simply hear better is the major topic of the researchers in the Lower Saxony Cluster of Excellence "Hearing4all". Hannover Medical School (MHH) is focusing on improvements to hearing implants.
One example: cochlear implants are an established technique for helping people with moderate to complete hearing loss. The electronic hearing prosthesis is surgically embedded in the skull bone behind the ear. "The most challenging step is to insert the attached electrode into the sensitive structure in the inner ear so that it then hangs freely in the cochlea," reports research group leader Thomas Rau. This has to be done very carefully.
This is because a minimal injury could result in the patient losing their residual hearing. "Some patients therefore decide against an operation," says employee Georg Böttcher-Rebmann.
Until now, surgeons have had to rely on their instincts when inserting the thin and flexible electrode. However, the resistance they have to react to can hardly be felt. Georg Böttcher-Rebmann has developed a tool with a force sensor that measures the forces acting on the implant. The prototype is now being tested in a clinical trial with patients.
The "Hearing4all" Cluster of Excellence is led by the University of Oldenburg, with the MHH and Leibniz University also playing a major role. In Hanover alone, 15 working groups are conducting research directly in the network, with others cooperating. At Leibniz University, for example, chemists are developing coatings for cochlear implants that store anti-inflammatory drugs and release them after surgery.
The federal and state governments have been paying 55 million euros for seven years since 2019, 23 million of which will go to Hanover. MHH has also raised almost 15 million euros in additional funding since then.
Source reference: HAZ from 02.04.2024, page 11
Picture: Tim Schaarschmidt

We have put together an interesting program for you. You will accompany our researchers into their laboratories and learn, for example, how light gets into cells or how cells can help deaf patients. You will also find out how blood can be better preserved and how orthopaedic implants are researched.
All places have now been allocated!
Our Future Day activities are aimed at both girls and boys and are held in German. An additional offer is aimed exclusively at Ukrainian pupils and is held in Ukrainian.

Working groups from the Lower Saxony Center for Biomedical Engineering and Implant Research were present at the Health Weeks in Aufhof to give citizens an insight into their research work and impart knowledge. Through interactive presentations and informative discussions, the working groups succeeded in making the complex topic of biomedical engineering and implant research understandable and tangible. Visitors had the opportunity to find out about the latest developments and technologies and ask questions, resulting in a lively exchange between scientists and the public. The event helped to emphasize the importance of these research areas for people's health and well-being and to promote understanding of them among the general public.

Cover picture: ©Karin Kaiser/MHH


On 30.1.24 the 3rd event in the series 'Digital Implant Innovation Forum' took place very successfully at the NIFE, an event with 12 lectures on all aspects of tissue engineering (TE) as well as poster publications by individual groups in and around the NIFE.
Prof. Holger Blume and Prof. Meike Stiesch were present on behalf of the NIFE Board of Directors, while the President of the MHH, Prof. Manns, gave a welcoming address at lunchtime, emphasizing the multidisciplinary research work of the NIFE and in particular its value for the high-quality training of young female scientists. The TE is ultimately subject to the same "harsh conditions" as human or animal transplants, with high quality requirements in terms of function, strategies for maintaining function and immunological compatibility in the recipient. The event, which was very successful and packed with presentations, also covered topics from basic research on new possibilities for autologous cell harvesting and expansion from various body cell niches and immunogenic masking to prevent rejection, as well as very innovative possibilities for oxygen or pH monitoring in or on tissue, and completely new implant concepts such as carbon nanotubes for heart muscle support or energy harvesting in the body. Some of the new developments presented could potentially enable a quantum leap in the manufacture of implants, such as high-resolution 3D printing in scaffold production, supported by technical developments at bioprinter manufacturers and intelligent engineering innovations. The research team at NIFE came into close contact with other researchers from LUH and MHH as well as TU Dresden and with representatives of smaller and larger companies. In an exciting panel discussion, they discussed how results from TE research activities in Germany and Europe can be quickly transferred to industry and clinical applications and what hurdles, including financial ones, need to be overcome. Finally, the invited panelists were asked to summarize their motivation for the transfer of new TE products to industry and clinics for the R&D community. The following quote from Dr. Teepe, CellTro, (spin-off, Dresden) was a good example of this "Think big - and never give up!".



We are looking forward to the next event in this series, which is planned for fall 2024.

Man receives customized 3D-printed implant that also delivers medication
For the first time, the ENT clinic The team at Hannover Medical School (MHH) provided an adult patient with a customized implant for the external auditory canal. The implant is manufactured using 3D printing and is also designed to continuously and locally release an active ingredient to accelerate healing. "We have thus opened the door to innovative and pioneering patient care," explains ENT Clinic Director Professor Dr. Thomas Lenarz. The MHH is the first clinic in the world to produce an implant adapted to the patient's individual anatomy using the Desktop Health 3D bioplotter and to functionalize it by adding active ingredients.
The patient now fitted with the implant suffered from a recurring narrowing of the ear canal, which had been surgically treated several times without the desired success. The specially manufactured implant now enables both a stent function and drug delivery. "The first follow-up has already been very promising," reports PD Dr. Verena Scheper, whose team at the ENT Clinic's Pharmacology of the Inner Ear department designed the implant and manufactured it using the 3D bioplotter Manufacturer Series.

This treatment is an individual treatment attempt, as the patient has not been treated with conventional options. Funding is provided by the motivated ENT clinic.
The ENT Clinic at the MHH is internationally renowned for the world's largest cochlear implant program for the care of patients with hearing loss. The first CI operation was performed here in 1984. The German Hearing Center Hannover was opened in 2003. To date, the clinic has provided more than 11,111 patients with cochlear implants. The clinic also specializes in the provision and further development of hearing aids, the early detection of childhood hearing loss and the diagnosis and treatment of sensorineural hearing loss, including tinnitus.
Text: Daniela Beyer
Published under: https://www.mhh.de/presse-news/mhh-setzt-weltweit-erstes-innovatives-implantat-in-gehoergang-ein

As part of this year's Knowember der Wissenschaft, NIFE and the SIIRI Collaborative Research Center organized an interesting journey through the fascinating world of biomedical engineering and implant research. Visitors experienced insightful insights, immersed themselves in innovative research projects and learned more about the latest developments in the field. The event was extremely successful and the positive feedback from participants reflects the enthusiasm for the groundbreaking work of the researchers at NIFE.
We are looking forward to the Knowember of Science 2025, NIFE and SIIRI will be there again!



On 02.11.2023, the event took place for the second time OrthoRetreat took place at the NIFE under the title "Orthopedic Implants and Surfaces". Research approaches relating to osteoarthritis, the reconstruction of tendons and ligaments as well as patient-specific therapeutic approaches were presented and discussed. The exchange between basic science-oriented researchers with a view to cellular reactions and their pathological correlations and clinicians who face the challenges of individual patients on a daily basis was particularly valuable. This revealed new therapeutic approaches that are producing promising results in initial studies, but whose principles are not yet fully understood and need to be researched in greater depth. The medical and biomedical engineering students in attendance were also able to gain an insight into how clinical issues are viewed from different perspectives and how possible solutions are jointly developed. This valuable exchange was deepened during networking over finger food and drinks and further specific challenges were discussed and new ideas developed together.


On Thursday, October 12, 2023, this year's kick-off event of the TRAIN Academy took place at NIFE. A total of 19 scientists from the Hannover-Braunschweig-Göttingen region will take part in the extra-occupational training "Translational Research and Medicine: From Idea to Product" of the Translational Alliance in Lower Saxony over the next 24 months. Within the scope of the further education, you will expand your knowledge around biomedical product development.
The kick-off event also saw off the graduates of previous years who completed the program. Seven of them were present in person and were able to receive their graduation certificates.
This year, the key note lecture of the kick-off event was held by Prof. Josef Penninger, new Scientific Director of the Helmholtz Centre for Infection Research in Braunschweig since July 2023. The afternoon at NIFE was rounded off with a get-together of the approximately 50 attendees.


From November 6 to 8, the "International Conference on Biomedical Technology" will take place in Hannover. More information is available here.
On Sept. 16, 2023, Prof. Dominik Egger from the Institute of Cell Biology and Biophysics at Leibniz Universität Hannover gave an exciting lecture on the topic of innovative cell culture techniques.
The talk covered several key topics, including 3-D isolation of stem cells, the use of stem cells and stem cell products as drugs, and the development of 3-D cell culture models and their application in drug testing.
We are excited to see how these techniques will revolutionize medical research and treatments in the years to come.
Prof Egger is at your disposal for any questions you may have
Prof. Dr. Dominik Egger
Institute for Cell Biology and Biophysics
30419 Hanover
Egger(at)cell.uni-hannover.de


On 11.09.23 - despite high summer temperatures - the 2nd event of the Digital Implant Innovation Forum, which is under the auspices of the Digital Health City Hannover and the NIFE, attracted more than 100 interested people to the NIFE.
The DIIF Forum is dedicated to promoting expert:ing exchange and innovation in the field of smart and precision implants and digitalization in medicine.
The 2nd event, "Next Generation Individualized Patient Solutions by Additive Manufacturing," was all about 3D printing as an ideal platform for personalized implant design such as customization to individual patient anatomy.
The audience was treated to exciting technical presentations ranging from high-performance materials for additive manufacturing to biocompatibility of 3D printed constructs and the use and limitations of AI.







In the afternoon, the Translational Center for Precision Medicine was presented in the presence of Frank Doods, State Secretary of the Lower Saxony Ministry of Economics, Transport, Building and Digitalization, Prof. Michael Manns, President of the MHH, and Prof. Holger Blume, Vice President of the LUH.
The planned translational center is a unique project in Germany that Hannover Medical School is planning together with the NIFE research center and medical technology companies. A translational hub will comprehensively connect the clinics with basic research and the production of implants, so that patients can be supplied individually, quickly and with novel implants from the 3D printer.
An estimated 1 million people in Germany alone receive an implant every year, and demand is rising in the wake of demographic change. By personalizing implants, their so-called "service life" (i.e. functional life in the patent) can be extended and even rehabilitation times shortened. This is made possible by the rapid advances in the field of biomaterials and additive manufacturing.
In summary, the 2nd event of the Digital Implant Innovation Forum (DIIF) lecture series was also a great success and facilitated an excellent exchange between experts from different disciplines. The diverse discussions and presentations have opened up new perspectives. We would like to thank all participants, speakers and organizers for their contribution to this successful event. We are already looking forward to the next DIIF Symposium, which is expected to take place in December 2023 at NIFE and will provide a new opportunity to exchange knowledge and ideas.


# 1 Sensor technology for medicine and implants of tomorrow
On June 21, 2023, the kick-off event of the Digital Implant Innovation Forum under the auspices of the Digital Health City Hannover took place at NIFE.
The forum, which is dedicated to promoting the exchange of experts and innovations in the field of intelligent implants and digitalization in medicine, attracted around 100 experts to the NIFE despite the summer temperatures.
The event started with inspiring greetings from Prof. Windhagen, Executive Board NIFE, who warmly welcomed the participants and particularly emphasized the importance of sensor technology for the further development of implants and medical applications. This was followed by Prof. Bengel as Dean of Research at MHH, who emphasized the importance of the NIFE research center as a focal point of the Medical School. Mrs. Petersen from hannoverimpuls rounded off the greetings by showing how hannoverimpuls makes targeted economic development possible through clever promotion and support.
This was followed by a series of lectures and a discussion in which the experts presented their latest findings and experiences in the field of intelligent implants. They also discussed the often rocky road from the idea to practical application and the associated challenges. The speakers emphasized that innovation in this field not only requires technological know-how, but also has to take into account regulatory aspects, ethics and data protection.
Also discussed were the benefits of digital health applications, such as remote monitoring of implants, personalized medicine and improved patient care. At the same time, however, the associated challenges such as data security and privacy were also highlighted.
In summary, the launch event was a great success. It provided a platform for the exchange of knowledge, ideas and experiences. The interdisciplinary character of the forum enabled a holistic view of this exciting topic and promoted the dialog between experts from different disciplines.
We are already looking forward to the follow-up event, which will also take place at NIFE on 11.09.2023. You will find more information about it on our site soon.


On June 14 and 15, 2023, the first event organized by the German Society for Implant Research and Development (DGIFE) took place at the NIFE. Doctoral students from NIFE in the early phase of their scientific work were invited. The lecturers Prof. Claudia Neunaber, PD. Dr. Janin Reifenrath and Dr. Henning Voigt worked with the participants on the basics of scientific work, experimental design and publication of results. The interactive character of the event was rated particularly positively by the participants.



On 30.06.2023 the 2nd Science Day of the Department of Trauma Surgery took place at NIFE. The research day was a great opportunity to exchange information about the latest developments and advances in trauma surgery.The different working groups of UCH presented their latest research results and findings to their colleagues.The research day helped to further strengthen our knowledge and skills and to promote collaboration between the different areas of trauma surgery. Furthermore, the day offered an excellent opportunity to establish new contacts and to expand existing networks.
We look back on a productive day of research and look forward to our 3rd Science Day to be held in the spring of 2024.
Your Prof. Stephan Sehmisch

Samuel John, CEO at OtoJig GmbH opened the event with a presentation on the role of artificial intelligence as a tool for everyday life, science and medicine.
John presented examples of how AI can be used in medical imaging. By using algorithms based on machine learning, physicians and researchers can gain valuable information and make informed decisions. In hearing research, he said, this could help in the treatment of patients, particularly by improving minimally invasive surgical techniques for cochlear implantation. In addition, AI could also play an important role in the development and improvement of medical devices, such as hearing aids.
Next, Prof. Dr.-Ing. Waldo Nogueira presented his research findings on the application of AI to speech understanding in noisy environments for cochlear implant users. He explained that conventional cochlear implants have difficulty understanding speech effectively in environments with a lot of background noise.
He notes that AI algorithms could offer a promising solution to overcome these problems. By using neural networks, AI can analyze background noise and better separate the speaker's speech from background noise. This would allow cochlear implant wearers to better understand speech and participate in conversations even in noisy environments.
Both presentations offered an insightful look at advances in the field. Both Samuel John and Prof. Nogueira showed how AI can contribute to improvement in medical research.
The congress began with greetings from the 1st Chairman of ISPO Deutschland e.V., Michael Schäfer, who warmly welcomed the participants and gave a brief overview of the coming days. In the following days, numerous lectures were held by renowned scientists and researchers who presented their research results and experiences on the topic of amputation and prosthesis care.
Special highlights were the lectures by PD Dr. Alexander Gardetto from Italy on the "Feeling Prosthesis" and the Key Note Lecture in the evening by Prof. Rickard Branemark on Bionic Reconstruction Concepts in the historic Old Town Hall of Hannover. The crowning finale of the scientific congress program was provided by the cooperation partners of trauma surgery from Boston: Corey L. Sullivan (Brigham Hospital, Harvard Medical School) and Michael Fernandez (MIT) impressed the auditorium with their lecture on "Reinventing Amputations". The subject was the "AMI technique" , which was developed by Prof. Hugh Herr (MIT) and Prof. Matthew Carty and which is currently offered in Europe exclusively at the MHH.
The presentations were accompanied by lively discussions and a lively exchange between the participants.
On Friday, in addition to the lectures, there was also a series of workshops where participants could learn practical skills. The workshops were very popular and offered participants a valuable opportunity to expand their knowledge and skills "hands-on".



Overall, the ISPO Annual Congress was a great success. Participants were enthusiastic about the content presented and the opportunities for exchange and networking. The congress once again underscored the importance of amputation and prosthetic care to medical practice and patient care, and inspired participants to continue to work enthusiastically to improve amputation and prosthetic care.
For more information please contact
Jennifer Ernst, MD
Specialist for plastic and aesthetic surgery
Advanced Clinician Scientist Group Leader MOBILISE-Lower Saxony
Trauma Surgery Clinic
(Director: Prof. Dr. Stephan Sehmisch)
Hanover Medical School
Carl-Neuberg-Str. 1
30625 Hanover
Email: Ernst.Jennifer(at)mh-hannover.de

People born deaf use parts of the auditory brain area for vision. However, this does not hinder the recovery of the sense of hearing, MHH researchers found.
Humans have five senses to perceive their surroundings: Sight, hearing, touch, smell and taste. If a person loses one of these, the remaining senses partially compensate for the loss. People born deaf then have enhanced visual abilities. "Crossmodal plasticity" is what science calls the brain's ability to turn to another sensory system when one is lost. Until now, the textbook view has been that a takeover of the auditory system occurs in deafness, with the visual system, for example, irrevocably taking over parts of the auditory cortex. To avoid promoting this effect, some researchers have suggested avoiding communication through gestures or signing with children born deaf before the insertion of a hearing prosthesis such as the cochlear implant (CI).
Now, a German-American team of authors with Professor Dr. Andrej Kral, Scientific Director of the Institute for Audio and Neurotechnology (VIANNA) at Hannover Medical School (MHH), has compared recent data and studies from their own laboratories with others. These data show that crossmodal reorganization changes little in the anatomy of circuits in the brain. The existing networks are just used differently. When hearing is restored, the crossmodal reorganization regresses. The results are published in the journal Trends in Neurosciences been published.
During hearing, sound is converted into electrical impulses in the inner ear and transmitted via the auditory nerve through the midbrain and diencephalon to the cerebral cortex. This is where the auditory cortex is located, which is responsible for processing acoustic stimuli. Deaf people use parts of the auditory processing center in the cerebral cortex for visual impressions, such as motion detection. "Reorganizing the brain is helpful for deaf people to better navigate the environment without an auditory sense," says Professor Kral. "But contrary to earlier assumptions, the neural connections to the auditory sense are not destroyed, so the auditory cortex does not become a battleground between the remaining senses. The existing network is slightly altered and used differently."
This is shown by recent data from animal models as well as from deaf children with hearing loss. Rather, crossmodal reorganization is a dynamic process that makes greater use of already existing nerve connections to other sensory systems, takes place even with mild hearing loss, and regresses after hearing is restored, he says. "Therefore, there is no reason to stop visual communication before inserting a hearing prosthesis," the scientist emphasizes. "This is important for the child's development."
Nevertheless, rapid insertion of a CI is critical in children born deaf. Hearing loss has extensive negative effects on the auditory system itself that cross-modal reorganization cannot compensate for. "Early therapy with a CI is necessary because in congenital deafness, the hearing system itself cannot develop normally," Professor Kral explains. "If a child misses out on early hearing experiences, he or she loses many contact points in the auditory cortex and later fails to learn to recognize auditory impressions and speech sounds and to integrate hearing with other sensory perceptions." Therefore, he said, a hearing prosthesis must be inserted as early as possible, preferably in the first year of life, and at the very latest by age three. "After that, the critical period for hearing therapy is closed."
The original work "Crossmodal plasticity in hearing loss" can be found at. here.
Source: MHH, as at: 03 May 2023
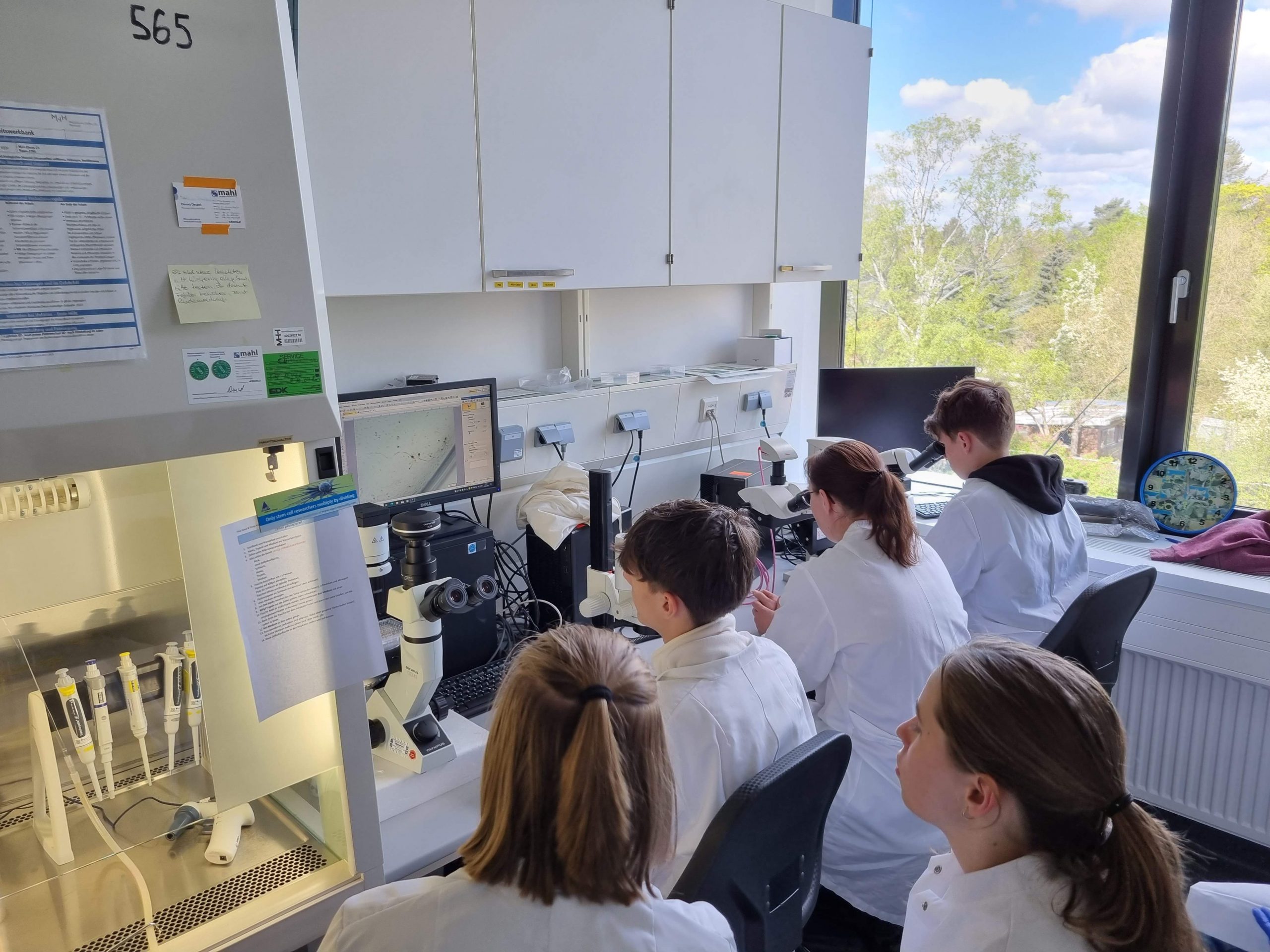
On 27.05.2023 28 children participated in the Girl`s and Boy`s Day at NIFE. The day was a great success! The children had the opportunity to work with our scientists and experience research first hand.
The students were able to gain an insight into everyday life and the workings of research in the laboratory.
The children learned many important tools and techniques themselves, tried their hand at pipetting, worked with cell cultures and evaluated samples under the microscope. With a lot of enthusiasm, the children have visited different work groups and learned about a wide variety of implants. In the laboratory, the students learned how to cryopreserve cells and examine biofilms.
Some students were also allowed to conduct listening tests at different sound frequencies in an anechoic chamber, a special laboratory room for acoustics experiments where almost no sound is reflected.
The children showed great interest in our research projects and asked many smart questions. We hope that they were inspired by this day and may even have the desire to work in research themselves one day, We look forward to the next generation of researchers and developers.


On 14.03.23 the kick-off event for the new lecture series "Safe implants for the future" of the Transregio Collaborative Research Center SIIRI took place at NIFE.
The event is aimed particularly at the interested public as well as clinicians and scientists and aims to explain complex scientific relationships in an understandable way.
Prof. Dr. Meike Stiesch explained to the audience what medicine can learn from aviation, Prof. Dr.-Ing. Stefan Zimmermann explained ion mobility spectrometry to the participants in a clear and understandable way and finally Prof. Dr.-phil. Christoph Klimmt explained to the audience why good communication is important in patient care. After the lectures, the participants had the opportunity to ask questions and exchange ideas with the experts. Finally, the participants were given the opportunity to experience research "live and hands-on" during a laboratory tour.
Overall, the first event of this lecture series was a complete success and successfully contributed to bringing implant research closer to a broad audience and raising awareness of the importance of this complex field of research. We are looking forward to the follow-up event to be held on March 21, 2023 at 6:00 p.m. in Lecture Hall P of the Dental, Oral and Maxillofacial Clinic of the Medical School on the topic: "Modern from head to toe: How we improve your care with innovative concepts!" and to which we cordially invite you already now.
Registrations are requested under SIIRI@mh-hannover.de .


